Hemorrhoid Artery Embolization (HAE)
What Are Hemorrhoids?
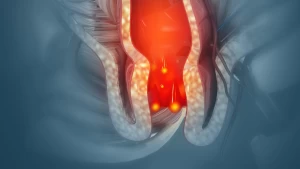
Hemorrhoids are swollen blood vessels in the lower rectum and anal canal. They can cause bleeding, itching, pressure, discomfort, and pain, especially during or after bowel movements. Hemorrhoid artery embolization is typically used to treat internal hemorrhoids, which form inside the rectum.
Who Is at Risk for Symptomatic Hemorrhoids?
Hemorrhoids are common in adults. Anything that increases pressure in the lower rectum can contribute, including:
- Straining during bowel movements
- Chronic constipation or diarrhea
- Pregnancy
- Obesity
- Prolonged sitting
Many people improve with diet and lifestyle changes. When symptoms persist, become disruptive, or include ongoing bleeding, a medical evaluation is important to confirm the cause and discuss treatment options.
How Are Hemorrhoids Traditionally Treated?
Treatment often starts with conservative care, such as increasing dietary fiber, staying well hydrated, and using stool softeners or topical medications. If symptoms continue, office-based procedures (like rubber band ligation, sclerotherapy, or infrared coagulation) may be recommended.
For severe or persistent cases, surgery (hemorrhoidectomy) has been a traditional option. Surgery can be effective, but it may also involve more post-procedure pain and a longer recovery.
What Is Hemorrhoid Artery Embolization (HAE)?
Hemorrhoid Artery Embolization (HAE), sometimes called the Emborrhoid technique, is a minimally invasive, non-surgical procedure that reduces blood flow to the vessels that feed internal hemorrhoids. By decreasing the blood supply, hemorrhoid tissue can shrink over time, and symptoms, especially bleeding, may improve.
HAE does not involve incisions in the anal area. It is performed through a small puncture in an artery, most often in the wrist or groin.
How Is the Procedure Performed?
HAE is performed by a vascular and interventional radiologist using live X-ray guidance (fluoroscopy). In general, the procedure includes:
- Sedation and comfort: Local anesthetic is used at the access site, and many patients receive moderate (“twilight”) sedation.
- Access: A tiny puncture is made in the wrist (radial artery) or groin (femoral artery).
- Catheter guidance: A thin catheter is guided through the arteries to the vessels supplying the hemorrhoids.
- Embolization: Small embolic materials (often coils and/or tiny particles, depending on your anatomy and treatment plan) are placed to reduce blood flow.
- Completion: The catheter is removed, and the access site is closed and bandaged.
How Long Does the Procedure Take, and Will I Go Home the Same Day?
Most HAE procedures take about 1–2 hours. Patients are typically monitored for a few hours afterward and go home the same day. You will need someone to drive you home if sedation is used.
Am I a Good Candidate for HAE?
HAE may be considered for patients with internal hemorrhoids that:
- Cause significant or recurrent bleeding
- Have not improved with conservative care (diet, fiber, topical treatments)
- Require a non-surgical option due to personal preference or medical considerations
Candidacy is determined through a consultation and review of your symptoms and medical history. Your care team may also recommend an evaluation to rule out other causes of rectal bleeding.
What Are the Benefits of HAE?
Compared with more invasive surgical options, HAE may offer:
- A minimally invasive approach with no anal incisions
- Less post-procedure discomfort for many patients
- Same-day (outpatient) treatment in most cases
- Gradual improvement in bleeding and hemorrhoid-related symptoms as tissue shrinks
- Preservation of normal anal anatomy and sphincter function
What Are the Risks and Possible Complications?
HAE is generally considered safe, but all procedures carry some risk. Potential side effects and complications can include:
- Mild pelvic or rectal pressure, cramping, or discomfort
- Bruising, soreness, or bleeding at the wrist/groin access site
- Temporary changes in bowel habits
- Infection (uncommon)
- Reaction to contrast dye or temporary strain on kidney function (uncommon)
- Rare non-target embolization affecting nearby tissue
Your radiologist will review your specific risks with you, including any risks related to your medications and medical history.
What Should I Expect After the Procedure?
Many patients return to normal daily activities within 1–2 days, depending on how they feel and what type of access was used. Symptom improvement is typically gradual. Some patients notice bleeding improves sooner, with continued improvement over the following weeks as hemorrhoid tissue shrinks.
Your provider will give you specific aftercare instructions and follow-up recommendations. In some cases, additional hemorrhoid treatments may still be recommended depending on your symptoms.
Is HAE Covered by Insurance?
Coverage varies by plan and medical indication. Our team can help verify benefits and determine whether prior authorization is required before scheduling.
Can the Procedure Be Repeated?
In some cases, embolization can be repeated if symptoms recur or if additional treatment is needed. Your interventional radiologist will discuss whether repeat treatment makes sense for your situation.
Schedule a Consultation
If you are experiencing persistent hemorrhoid symptoms, especially recurrent bleeding, and haven’t found relief with conservative care, a consultation can help determine whether Hemorrhoid Artery Embolization is an appropriate option.